18A138
Synovial Phenotype is Associated With Patient Biometrics in Inflammatory Arthritis
Author(s)
Candice Low1, Richard Conway1, Francis Young1, Monika Biniecka1, Hannah Convery1, Kieran Murray1, Ursula Fearon2, Douglas Veale1
Department(s)/Institutions
1. Centre for Arthritis and Rheumatic Disease, St. Vincent’s University Hospital, University College Dublin, Ireland 2. Department of Molecular Rheumatology, School of Medicine, Trinity Biomedical Sciences Institute, Trinity College Dublin, Dublin 2, Ireland
Introduction
The potential importance of altered body composition in the development of and disease course in inflammatory arthritis is increasingly being recognised. Body composition in different types of inflammatory arthritis and its influence on synovial pathology remains to be fully characterised.
Aims/Background
To evaluate body composition in seropositive and seronegative rheumatoid arthritis (RA) and psoriatic arthritis (PsA) patients and assess associations with disease characteristics and baseline synovial arthroscopic findings.
Method
We performed a prospective observational study of consecutive inflammatory arthritis patients seen in outpatient clinics. Demographic and clinical characteristics were collected on all patients. Synovial biopsy was performed by needle arthroscopy, and macroscopic and histologic features recorded. The degree of synovitis and vascularity were recorded on a 0–100-mm visual analog scale, and chondropathy on a semi-quantitative scale from 0-3. Mann-Whitney U test was used to compare groups. Spearman’s Rank Correlation Coefficient was used to assess for associations between biometrics and demographic and clinical markers. GraphPad Prism Version 7 and IBM SPSS Statistics Version 24 were used for data analysis.
Results
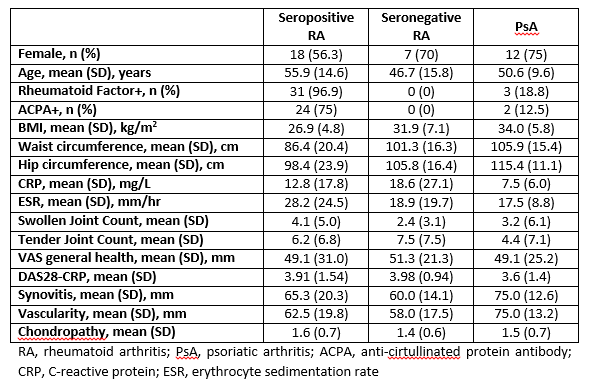
We included 58 patients, 32 with seropositive RA, 10 with seronegative RA, and 16 with PsA. 37 (64%) were female. Mean (SD) age was 52.8 (13.9) years. Mean (SD) BMI was 29.7 (6.3) kg/m2, waist circumference was 94.4 (20.3) cm, and hip circumference 104.3 (21) cm. Full demographic and clinical details are shown in Table 1. Seronegative RA patients had significantly increased BMI (p=0.033) and waist circumference (p=0.017), but not hip circumference (p=0.248) compared to seropositive RA patients. PsA patients had significantly increased BMI (p<0.0001), waist circumference (p=0.001), and hip circumference (p<0.001) compared to seropositive but not seronegative RA patients. There was a significant correlation between waist circumference and both synovitis (r=0.31, p=0.018) and vascularity (r=0.34. p=0.010) at arthroscopy. BMI and hip circumference did not correlate with arthroscopic findings.
Conclusions
Different types of inflammatory arthritis have distinct body composition profiles. Waist circumference, but not other biometrics, correlates with baseline synovial inflammation and vascularity.