ISR Autumn Meeting 2019
2nd Place Clinical Oral Presentation
Siobhan Clifford
19A142
The added utility of the EMA panel to the clinical and pharmacological management of suspected inflammatory conditions
Author(s)
Siobhan Clifford, Dr. Liam Chawke, Dr. Gráinne Murphy, Dr. John Ryan
Department(s)/Institutions
Department of Rheumatology, CUH
Introduction
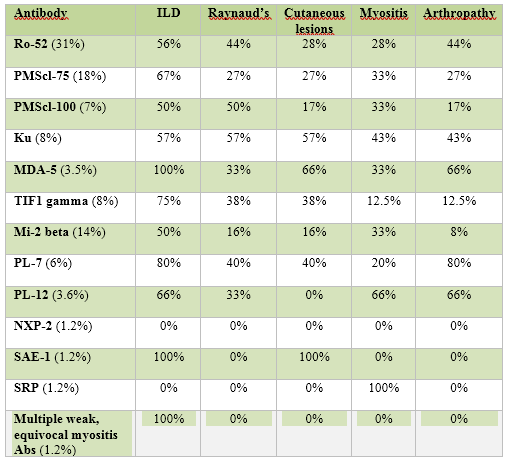
The idiopathic inflammatory myopathies are a rare collection of disorders primarily characterised by proximal muscle weakness sometimes accompanied by cutaneous manifestations, Raynaud’s syndrome, interstitial lung disease and arthropathy. The introduction of the EMA panel, testing for myositis specific and myositis associated antibodies (MSA/MAA) provides an additional mode of investigation which helps further refine inflammatory diagnoses and management.
Aims/Background
The objectives of the study are:
1. To determine the prevalence of autoantibodies from the EMA panel results
2. To identify disease manifestation of patients who have a positive EMA panel
3. To establish if the presence of certain autoantibodies alters a diagnosis or treatment
Method
This is a retrospective chart review of all Cork University Hospital patients who had a positive EMA panel test between January 2013 and June 2018. Data was obtained from CUH immunology lab archives along with individual patient charts and was compiled in a password protected Excel spreadsheet. SPSS version 24 was used to analyse the data.
Results
25.5% of 337 EMA panel tests during the specified time -frame were positive for one or more MSA/MAAs. Of those, 82 charts were available and analysed. The most prevalent antibodies were Ro-52 (33%), PMSCl-75 (18%), Mi-2a/b (15%) and TIF1-gamma (10%). The most common disease presentation was ILD at 57% followed by arthropathy with a prevalence of 30%. Raynaud’s and myositis were also common findings with a prevalence of 29% each individually. 28% experienced cutaneous manifestations. Following the EMA panel, 40% patients had their diagnosis changed or refined according to antibodies present. Of those who followed-up, 62% experienced an improvement in symptoms subsequent to medication alterations following EMA panel.
Conclusions
Use of the EMA panel may lead to a change in diagnosis for 40% patients thus leading to adjustment of treatment and improvement of disease manifestations. Despite only 29% presenting with clinical myositis, 39% patients went on to have a myositis-related diagnosis following EMA test further proving its use clinically. However, due to low prevalence of the IIMs, a longer-term study is required to precisely elucidate correlation between antibodies, diagnoses and treatment success.